How CCBHCs are transforming behavioral health

How CCBHCs are transforming behavioral health In just a few short years since the first Certified Community Behavioral Health Clinics (CCBHCs) opened their doors in 2017, the movement has revolutionized behavioral health in the U.S. This innovative model is delivering impressive results, dramatically increasing access to mental health and substance use disorder (SUD) treatment, expanding […]
Worklow mapping for your behavioral health organization | Tips and tricks
Workflow mapping for your behavioral health organization | Tips and tricks The second article in our content series titled Professional Services: Practices for Behavioral Health Organizations, highlights how Qualifacts’ OnCall Health professional services team, including our Professional Services Director and Solutions Engineers, can help your behavioral health organization better understand and drive efficiency in your […]
Technology should be part of your staff retention strategy: here’s why

Technology should be part of your staff retention strategy: here’s why Even as the pandemic wanes and the economy cools, behavioral health leaders rank staff recruitment and retention as top priorities. Years of labor shortages and surging patient demand have left organizations struggling to meet staffing needs. Astute leaders strive to take care of the […]
DEA telehealth changes | Everything you need to know

DEA telehealth changes | Everything you need to know The DEA proposed new rules in February 2023 in an attempt to balance safe prescription practices with the increasing dependence on remote healthcare providers- and the new guidelines seem to be a mix of pre-COVID and pandemic rules. To be clear, these new rules apply only when: […]
How to unlock mental health funding opportunities with Medicaid

How to unlock mental health funding opportunities with Medicaid If you’re considering how to scale your behavioral health business to reach more patients, you likely know that Medicaid is the single largest funder of behavioral health in the U.S. In fact, no payer in the U.S. funds more behavioral health services than Medicaid. Accounting for […]
Levelling up client engagement in behavioral health

Levelling up client engagement in behavioral health The pandemic reshaped healthcare delivery in ways we never imagined. It spurred rapid innovation in healthcare, with telehealth and technology emerging as indispensable tools for providing both physical and behavioral care. Now, clients expect a superior experience– to be involved in their care and engage with their providers […]
4 Patient Reported Outcome Measures that Lead to Better Business
4 Patient Outcome Measures that Lead to Better Business By measuring behavioral health outcomes, you can gain crucial insights to impact all areas of your organization. You can monitor patient progress, assess the effectiveness of interventions and treatments, and identify areas for potential improvements. Armed with better outcome measurements, you can improve communications between providers, […]
How the No Surprises Act affects your mental health agency

How the No Surprises Act affects your mental health agency The No Surprises Act, passed in 2022, was designed to protect consumers from unexpectedly high healthcare costs. Before the Act’s implementation, it was common for patients to be billed for non-covered costs during emergencies or when patients hadn’t approved out-of-network charges in advance. Consider, for […]
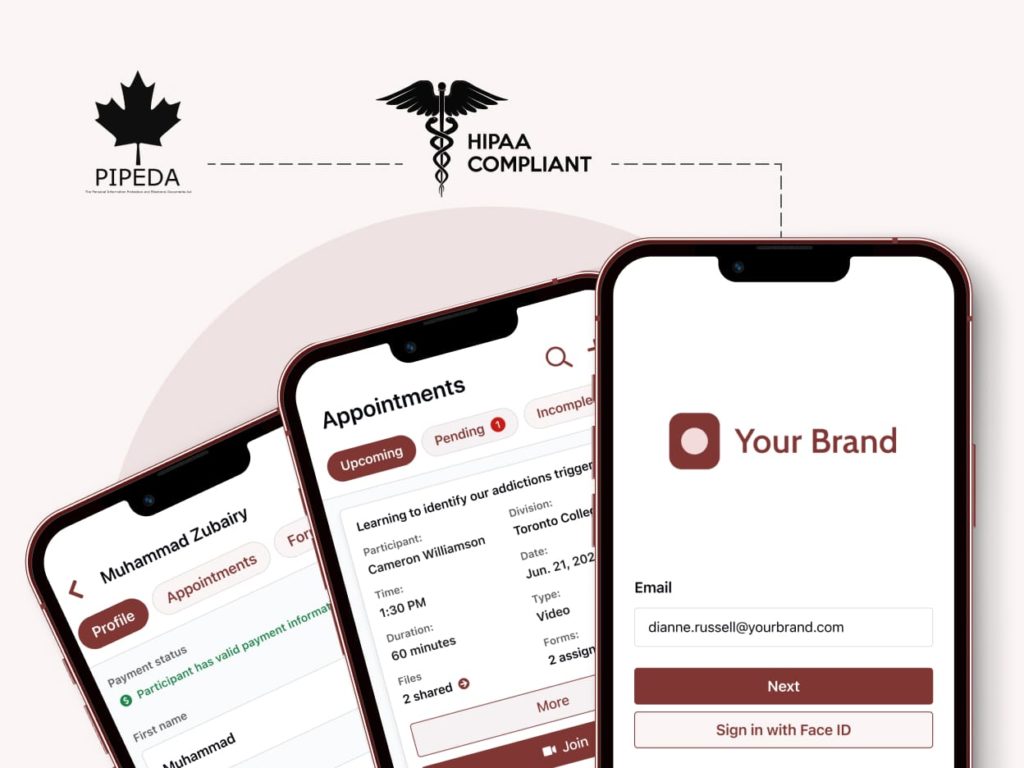
How to increase patient satisfaction with a white label telehealth portal

How to increase patient satisfaction with a white label telehealth portal Cultivating a gold-standard patient experience is essential in behavioral health. This is especially true as many patients, especially IDD (intellectual and development disabilities) patients, require additional resources and assistance throughout treatment. Although many behavioral health agencies see virtual care and a white label telehealth […]
Increase mental health funding for your organization: 4 tips

Increase mental health funding for your organization: 4 tips Our latest article, available on the Qualifacts website, looks at 4 ways your behavioral health organization can use telehealth and a patient portal to increase funding. We review how each of the following impacts your agencies funding: Care accessibility Work automations Compliance and transparency Value-based care […]
Elevating the IDD behavioral health experience with virtual care

Elevating the IDD Behavioral Health Experience With Virtual Care Our latest article, available on the Qualifacts website, highlights the different ways behavioral health organizations can use telehealth and a patient portal to close the gap in care for IDD (intellectual and developmental disabilities) patients. We review: The unique challenges associated with IDD care How reimbursement […]
How OnCall’s integration with CareLogic saved this leading behavioral health company over 50 hours in admin time
How OnCall’s integration with CareLogic saved this behavioral health company over 50 hours in admin time With over 16 subsidiary brands across 5 states, this leading behavioral health company has leveraged OnCall to deliver and manage virtual care programs since 2019. It was important that they had a sleek and easy-to-navigate patient portal that made […]
How to reduce administrative costs by up to 14% with a patient portal and telehealth software

How to reduce healthcare administrative costs by 14% with patient engagement software Administrators working for behavioral health companies have a wide range of responsibilities. They are often tasked with completing patient admissions and intake, data collection, insurance verification, and billing. Administrators work tirelessly to ensure providers are set up to complete appointments successfully, while also […]
5 reasons your behavioral health company needs a white label patient portal
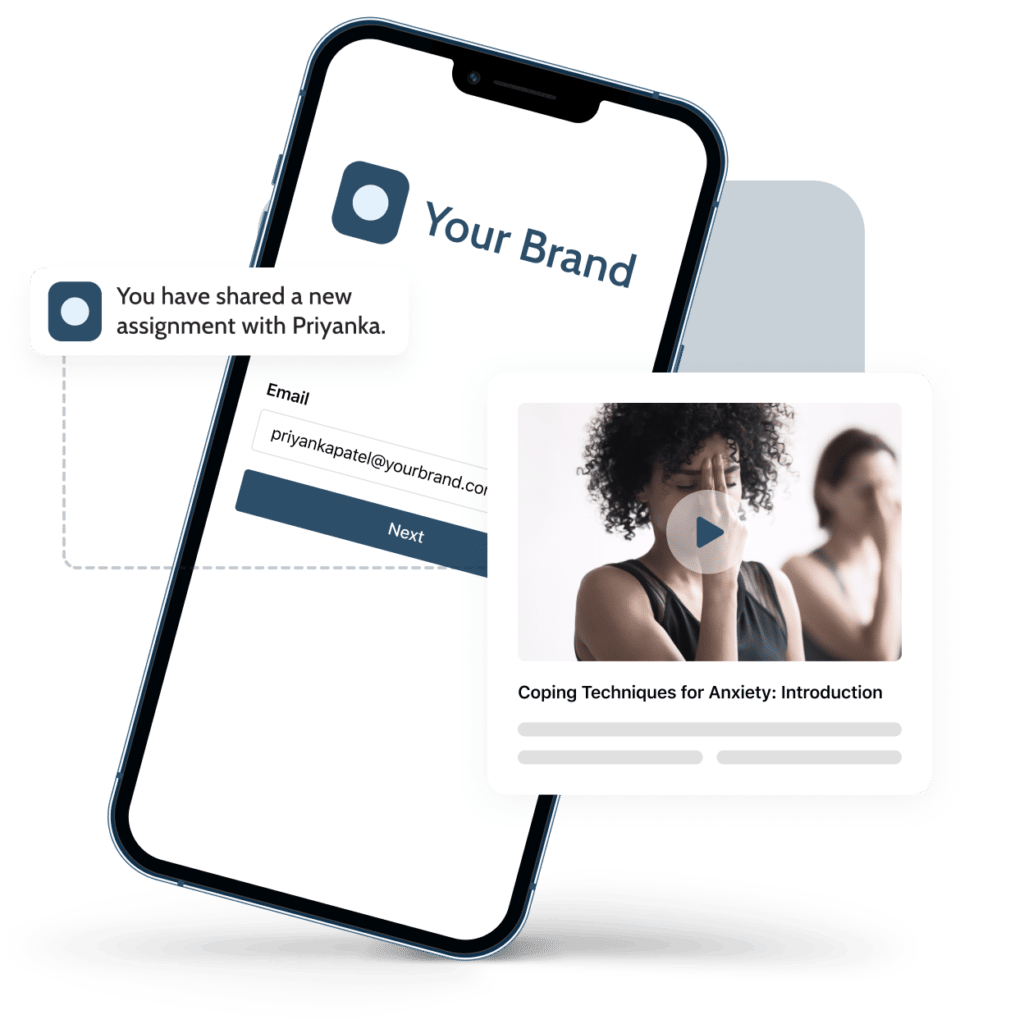
5 reasons your behavioral health company needs a white label patient portal What is a patient portal Unlike an EHR (Electronic Health Record), a white label patient portal designed for behavioral health is specifically created to enhance the patient experience, improve care quality, and boost clinical outcomes. While an EHR is designed to be provider-facing […]
OnCall’s 2022 Annual Telehealth Feature Roundup

OnCall’s 2022 Annual Telehealth Feature Roundup OnCall’s 2022 feature roundup highlights our product improvements and key features released this year. Our patient portal and telehealth solution continues to make it easier for behavioral health companies to deliver high quality care, and we’ve made improvements to make the software even better for you. With your feedback […]
Expanding behavioral health services: three telehealth use cases to consider in 2023

Expanding behavioral health services: three telehealth use cases to consider in 2023 Payers, policymakers, behavioral health companies, and providers are still working on rules for permanent adoption of telehealth and expanding successful telehealth programs to serve more clients and grow business. These stakeholders see the potential of telehealth to grow business while helping to meet […]
Tips & Tricks: Modern Marketing Practices for Behavioral Health Companies

Tips & Tricks: Modern Marketing Practices for Behavioral Health Companies The behavioral health market was estimated to be worth around $41 billion in 2021 and is expected to grow exponentially to $66 billion in the next 10 years. This tremendous growth, coupled with the behavioral health provider shortage and increased patient interest in mental healthcare, […]
5 tips to managing patient care during a stressful holiday season

5 tips to managing patient care during a stressful holiday season By OnCall Thought Leader Carrie Singer, Psy.D, Licensed Psychologist and Executive Director, Quince Orchard Psychotherapy What if December isn’t the most wonderful time of the year for everyone? Loneliness, stress, pressure, comparisons, financial strain, family dysfunction, and cold cloudy weather can all compound into […]
Telehealth trends for behavioral health in 2023: 4 key opportunities for growth

Telehealth trends for behavioral health in 2023: 4 key opportunities for growth By Nicholas Chepesiuk, CEO, OnCall Health For the last several years, we’ve witnessed a breathtakingly rapid digitization of behavioral health care. This was spurred by concessions made to allow use of technologies like telehealth, which are so crucial to the continued delivery of […]
How to Best Utilize Technology for High-Quality Care

How to Best Utilize Technology for High-Quality Care Demand for mental health support services and the use of telehealth for delivery has grown in popularity in the behavioral health space. In an effort to deliver high-quality, end-to-end care programs with increased access, more patient touch points, high engagement, and broad data capabilities, many organizations have […]
How OnCall’s onboarding team helped a leading behavioral health company increase virtual appointments by 200%

Identifying opportunities for growth In 2019, a leading U.S. behavioral healthcare company launched telehealth programming using over nine point products to serve patients in isolation due to the pandemic. Their administrative staff were incredibly strained, and providers were experiencing burnout due to the manual work associated with swiveling between so many products, copious amounts of […]
Leveling the behavioral health playing field: how telehealth software can increase employee engagement

Leveling the behavioral health playing field: how telehealth software can increase employee engagement Even before the pandemic, it was frustratingly hard to find, hire, and keep the best clinicians and administrative staff. With post-pandemic surges in mental health and substance use disorder issues and the complex set of challenges related to the Great Resignation and […]
4 ways a telehealth platform can help you navigate uncertainty and improve outcomes

4 ways a telehealth platform can help you navigate uncertainty and improve outcomes What’s next for telehealth is one of the most urgent questions for healthcare providers as the pandemic ends. Telehealth use for medical and behavioral health care soared during the pandemic, helping to ensure that patients continued to receive the care they needed […]
How your company can use data to improve clinical outcomes and boost patient care

How your company can use data to improve clinical outcomes and boost patient care Do you know the impact telehealth is having on your company? Measuring the strength of your telehealth programs and services is key to a successful long-term growth strategy. With this data you’ll be able to track the health of provider adoption […]
What Clinical Directors Should Know About Value-based Care for Behavioral Health

What Clinical Directors Should Know About Value-based Care for Behavioral Health Soaring medical costs and declining quality of care in the U.S. have led Medicare and insurers to look for alternative payment models such as value-based care (VBC), aiming to improve clinical outcomes for patients while reducing costs. VBC has demonstrated promising results, and models […]
OnCall Health Recognized As Software Advice Frontrunner in 2022

OnCall Health Recognized As Software Advice Frontrunner in 2022 OnCall Health is honored to announce its recognition as a Top Mental Health Software by Software Advice in its 2022 Frontrunners report. Software Advice is a leading company that helps businesses navigate their software buying journey. This report evaluates verified end-user reviews, positioning the top scoring products based on […]
One plan, many benefits: how you can increase behavioral health care access and outcomes with subscription services

One plan, many benefits: how you can increase behavioral health care access and outcomes with subscription services Building on the momentum of surging telehealth adoption in behavioral health care during the pandemic, leading behavioral health companies are now leveraging technology to re-imagine the future of care. Not only does technology help make care more accessible […]
The game-changer in reducing behavioral health provider burnout: three telehealth strategies you should adopt

The game-changer in reducing behavioral health provider burnout: three telehealth strategies you should adopt For behavioral health providers, burnout has always been a very real risk of an intensely focused and stressful job. Even before the pandemic, in 2018, the American Psychological Association estimated that up to 61% of mental health practitioners were experiencing burnout […]
3 ways virtual care is changing behavioral healthcare
3 ways virtual care is changing behavioral healthcare At the height of the pandemic, behavioral health companies were forced to implement technology and processes to continue caring for patients. The processes and platforms, which they continue to use, are disconnected, manual, and burdensome for providers, administrators, and patients alike. Staff continue to rely on disparate […]
Your top questions about telehealth integrations, answered

Your top questions about telehealth integrations, answered Interoperability in healthcare is crucial for continuity of care, to ensure providers have all the patient data they need at their fingertips to effectively and accurately provide care. However, interoperability and telehealth integrations are only just starting to become a priority for many behavioral health companies. Although behavioral […]
CHE Behavioral Health Services chooses OnCall’s telehealth solution to power its patient facing care programs

OnCall Health will enable CHE to continue its multi-state expansion throughout the USA. TORONTO, CALIFORNIA – May 26, 2022 – OnCall Health (OnCall) is proud to announce its recent client addition of CHE Behavioral Health Services (CHE), the gold standard in behavioral health in the United States. This partnership will expand accessibility to exceptional behavioral virtual […]
3 ways telehealth helps behavioral health companies maximize efficiency, retain patients, and increase revenue

3 ways telehealth helps behavioral health companies maximize efficiency, retain patients, and increase revenue Although behavioral health companies implemented technology and processes at the height of the pandemic to continue caring for clients, the processes they chose and continue to use are disconnected, manual, and burdensome for providers, administrators, and patients alike. Two years into […]
3 critical steps to scaling your telehealth operations

3 critical steps to scaling your telehealth operations At the height of the COVID-19 pandemic, behavioural health and addictions organizations were forced to leverage disparate systems as a short-term solution in order to continue caring for clients. Organizations quickly implemented different video conferencing solutions, charting software, and e-prescription platforms. The consequences of using disparate systems […]
The what and why of APIs for your addictions organization

The what and why of APIs for your addictions organization At the height of the COVID-19 pandemic, healthcare clinics and organizations were forced to leverage disparate systems as a short-term solution in order to continue caring for patients. Organizations quickly implemented different video conferencing solutions, charting software, and e-prescription platforms. The consequences of using disparate […]
3 critical steps to delivering the best virtual care patient experience

Investing in a better virtual treatment experience is critical for your staff. Here’s 3 reasons why. At the height of the COVID-19 pandemic, behavioral health and addiction organizations were forced to rapidly adopt point solutions to care for clients. Although their providers continue to leverage video conferencing solutions and manual processes to manage telehealth operations […]
Investing in a better virtual treatment experience is critical for your staff. Here’s 3 reasons why.

Investing in a better virtual treatment experience is critical for your staff. Here’s 3 reasons why. In 2022 and beyond, we expect to see addictions organizations move away from point products and manual, disconnected processes towards comprehensive telehealth solutions that enable them to deliver efficient virtual treatment. But, why do healthcare leaders need to rethink […]
Trying to scale your telehealth programs with just a video conferencing tool? Try again.

Trying to scale your telehealth programs with just a video conferencing tool? Try again. In 2022 and beyond, we expect to see addictions organizations move away from point products like video conferencing tools and manual, disconnected processes towards comprehensive telehealth solutions that enable them to deliver virtual addictions treatment at scale. But, why do healthcare […]
OnCall’s 2021 product video

OnCall’s key features released in 2021 This video highlights OnCall’s key features released in 2021 that enhance the patient and provider telehealth experience. In this video we’re review 5 key features and explain how they help maximize provider and administrator efficiency to save time and money, and improve the patient experience for better patient health […]
Top trends in 2022 for telehealth for behavioural healthcare

Top Trends in 2022 for telehealth for behavioral healthcare At the beginning of the COVID-19 pandemic, behavioral health and addiction organizations were forced to rapidly adopt point products to care for clients. Unfortunately, these organizations continue to use point products and manual processes to deliver care even as the pandemic shows no signs of slowing […]
How to stay PHIPA and HIPAA compliant throughout your API integration

How to stay PHIPA and HIPAA compliant throughout your API integration HIPAA and PHIPA compliance are major features of OnCall Health. Our platform uses a variety of technical processes (including end-to-end encryption, which you can read about here) for this purpose. When building an integration, it’s important that you take steps to avoid exposing protected health […]
Why a HIPAA compliant video conferencing tool is not a telehealth strategy

Why a video conferencing tool is not a telehealth strategy At the height of the COVID-19 pandemic, behavioral health and addiction organizations were forced to rapidly adopt point solutions, like video conferencing tools, to care for clients. Although their providers continue to leverage video conferencing solutions to manage telehealth operations and provide virtual programming, they’re […]
A Leader’s Perspective: How to Grow Virtual Care Programs
An Addictions Leader’s Perspective: Shane Saltzman on How to Launch and Scale Successful Virtual Outpatient Programs with Telehealth By Shane Saltzman, CEO of Trafalgar Addiction Treatment Centers Shane Saltzman, CEO of Trafalgar Addiction Treatment Centers, speaks to OnCall about Trafalgar’s experience scaling their virtual outpatient programs with OnCall’s solution. Shane’s leadership and experience showcases his expertise […]
Behavioral Healthcare Executive: How to ensure telehealth exceeds data security and privacy requirements

How to Ensure Telehealth Exceeds Data Security and Privacy Requirements By Nicholas Chepesiuk, for Psychiatry and Behavioural Health Learning Network November 1, 2021 Digital healthcare has made patient care more accessible and convenient, while opening up new business opportunities for healthcare organizations. However, I’m often asked by healthcare leaders: How do we create the best and most secure […]
Canadian Healthcare Technology: Effective virtual care must be easy to use for both clinicians, patients

Effective virtual care must be easy to use for both clinicians, patients By Nicholas Chepesiuk, for Canadian Healthcare Technology October 2021 At the height of the COVID-19 pandemic, healthcare leaders, systems, and organizations were forced to rapidly implement digital healthcare solutions to continue caring for patients. In fact, there was a 154 percent increase in telehealth […]
Trying to deliver the best patient telehealth experience with just video conferencing? Try again.

Building virtual treatment programs with just video conferencing? Try again. Time and time again, OnCall’s experts are tapped to help healthcare leaders implement successful telehealth systems so providers can deliver superior virtual treatment programs. Often, this includes comprehensive workflow development, integrating data-sharing technology, and preparing providers so they can deliver the best client experience. A […]
Top 5 ways complete telehealth solutions make your providers more efficient

Top 5 ways complete telehealth solutions make your providers more efficient Currently, most healthcare organizations leverage multiple, disconnected telehealth solutions to manage their virtual care operations and provide virtual treatment programs to clients. Their piecemeal infrastructure is made up of an EMR, a video conferencing tool, and perhaps unsecure email and phone to deliver comprehensive […]
How OnCall helps you deliver better telehealth for behavioral healthcare

Why you need more than point products to deliver virtual treatment programs? Healthcare organizations are using electronic medical records (EMRs), video conferencing tools, and other systems to deliver virtual treatment programs. Some come with healthcare tool add-ons, such as video conferencing and content management, but these features don’t deliver an end-to-end workflow, meaning that they […]
MedTech Intelligence: Connected telehealth systems lead the way for the future of healthcare

Connected Telehealth Systems Lead the Way for the Future of Healthcare By Nicholas Chepesiuk, for MedTech Intelligence July 22, 2021 As organizations continue to use technology to enhance the way they provide care, changes must be made to ensure the interoperability of the technology, patient data and continuity between providers. Telehealth has come a long way […]
Healthcare Business Today: Disconnected healthcare technology is a burden on all of us, and APIs can help

Disconnected healthcare technology is a burden on all of us, and APIs can help By Nicholas Chepesiuk, for Healthcare Business Today July 21, 2021 At the height of the COVID-19 pandemic, healthcare organizations were forced to leverage telemedicine as a short-term solution to ensure continuity of care for patients. As a result, patients have embraced telemedicine’s […]
The history of telemedicine and telemedicine trends

The history of telemedicine While the last few years have seen telehealth completely revolutionize the way patients interact with their healthcare providers – especially with the onset of the Covid-19 pandemic – telemedicine has actually been around for quite some time, dating back to the first half of the 20th century. Introduction of Telemedicine in […]
How to make sure your organization is PHIPA compliant

How to make sure your healthcare organization is PHIPA compliant Virtual care has seen a complete transformation as a result of the pandemic and now more than ever, patients and providers are turning to telemedicine to connect remotely and seamlessly using technology. But one of the more important components surrounding virtual care is PHIPA compliance – […]
Three ways telehealth solves for accessibility in healthcare

How does telehealth solve for accessibility challenges in healthcare? In the U.S., an estimated 25 percent of patients do not have access to a healthcare provider, particularly patients who live in rural areas. In Canada, because of an increase in provider shortages, patients can wait up to four weeks to see a provider. The lack of accessible […]
Canadian Healthcare Technology Magazine: Organizations making healthcare more effective with connected tech

Organizations making healthcare more effective with connected tech By Nicholas Chepesiuk, for Canadian Healthcare Technology Magazine, Vol. 26. No. 5, June/July 2021 At the height of the COVID-19 pandemic, healthcare clinics and organizations were forced to rapidly implement technology platforms as a short-term solution to continue caring for patients. While the solutions succeeded in connecting patients […]
Telehealth platforms are revolutionizing healthcare, but are they here to stay?

Telehealth platforms are revolutionizing healthcare, but are they here to stay? What happened to healthcare in 2020? Telemedicine’s exponential growth is felt and seen everywhere. Large healthcare organizations are leveraging telemedicine solutions to connect their technology, provide better healthcare delivery, and make providers more efficient. When the pandemic’s isolation restrictions have waned and as the […]
Pharmacy Practice & Business (Canadian Healthcare Network): Virtual care platform used to schedule vaccine appointments
Virtual care platform used to schedule vaccine appointments While some pharmacies bought new systems to handle COVID-19 vaccine bookings, DrugSmart pharmacies decided to use their existing virtual care platform to plan appointments. By Kylie Taggart, for Pharmacy Practice + Business (Canadian Healthcare Network) 16/18/2021 Pharmacies across Canada are using different booking software to deal with scheduling […]
OnCall Health rises to healthcare interoperability challenge with enhanced API

API securely connects OnCall’s telemedicine solution with third-party healthcare technology and data for greater efficiency and better health outcomes TORONTO – June 3, 2021 – OnCall Health today introduced an enhanced API (Application Programming Interface) with new functionality that seamlessly integrates its telemedicine solution with a healthcare provider’s existing technology to alleviate interoperability challenges that have long been identified as […]
Propelling public health forward with DrugSmart’s telehealth program

Introduction DrugSmart, an independent pharmacy coalition in Canada founded over 40 years ago, launched their Virtual Clinic program in 2020 with OnCall’s solution. Powered by OnCall, DrugSmart’s Virtual Clinic enables patients to meet with a pharmacist or physician online any day of the week through video conference or instant messaging. Since launch, DrugSmart has scheduled […]
What is an API and how does it benefit your behavioral health business?

What is an API and how does it benefit your telehealth platforms? How Can OnCall’s API increase interoperability between your telehealth platforms? Ranked as one of the leading digital health solutions in North America, OnCall’s API allows data seamlessly flows between your telehealth platforms and OnCall to reduce administrative redundancies, so providers can be more […]
Demystifying APIs for behavioral health companies

Demystifying APIs for telemedicine solutions At the height of the COVID-19 pandemic, healthcare clinics and organizations were forced to leverage disparate telemedicine solutions as a short-term solution in order to continue caring for patients. Organizations quickly implemented these solutions, such as video conferencing, charting software, and e-prescriptions platforms. The consequences of using disparate telemedicine systems […]
The Canadian Mental Health Association: The advantages of attending peer group meetings online

One peer’s story of the rich experience of embracing virtual care at CMHA Ottawa Article originally appeared on the Canadian Mental Health Association’s website – Every Wednesday before the COVID-19 pandemic, Robert used to hop in his car and attend an in-person peer support group at CMHA Ottawa. On the way, he would stop at Tim […]
Which telehealth platform is right for your healthcare company?

Which telemedicine platform is right for your healthcare organization The global telemedicine market was valued at $24.9 billion dollars in 2016 and is expected to reach $113.1 billion dollars by 2025. With telemedicine platforms, providers are empowered to think about healthcare outside of the walls of their clinics and organizations, so they can provide care […]
OnCall Health attests its virtual care platform meets mandatory requirements for virtual visit verification

OnCall Health is now one of only four vendors currently listed as verified virtual visit solution providers TORONTO – (BUSINESS WIRE) – Ontario Health has established mandatory requirements as part of the provincial standard for Virtual Visits Verification solutions for use within the Ontario health care sector. OnCall Health has attested that it and its virtual care […]
The Globe and Mail: Meeting urgent healthcare needs with virtual solutions

Original article published in The Globe and Mail Medical Innovation Special Report on February 18, 2021. For more than six years, Toronto-based Trafalgar Addiction Treatment Centres hosted once-a-week aftercare therapy sessions for clients enrolled in its addiction rehabilitation programs. So when COVID-19 threatened the continuity of these much-needed sessions, Trafalgar’s CEO reached out to virtual care solutions provider OnCall […]
Welcome to the new OnCall Health!
Today, we at OnCall are excited to announce our new and exciting look. We’ve refreshed our logo, branding, and website to showcase OnCall’s evolution from a simple, secure healthcare video conferencing solution to a complete virtual care program management platform for clinics and enterprises. Virtual care has grown over the last few years and exponentially […]
Dylan Zambrano grows DBT Virtual with OnCall

OnCall helped Dylan Zambrano launch and grow his mental health virtual care practice Dylan’s OnCall story begins in 2016 as a newly graduated therapist hoping to quickly start his own practice. He looked for a solution that would allow him to make Dialectical Behavior Therapy (DBT) accessible but that kept his bottom line in-check. Dylan’s […]
Top telehealth trends in 2021

Top trends in telemedicine in 2021 Virtual care has grown by 240% in Canada since April 2020, with 45% of clinicians choosing to implement telemedicine services into their practice. 1 in 4 Americans have used telemedicine services during the pandemic, and the use of telemedicine has increased ten-fold in China since March 20203. Although telemedicine […]
Virtual care eases access to mental health and addiction services

Original article published in Canadian Healthcare Technology Magazine, VOL. 25, NO. 8, November/December 2020 By Nicholas Chepesiuk We are at a crossroads in mental healthcare. The pandemic is leading us to either turn a blind eye to the growing wave of mental illness and addiction in Canada or use the circumstances as an opportunity to […]
HVE Healthcare Assessments turns to virtual care for insurance claim evaluations

Pandemic reinforces the benefits of virtual medical assessments in validating insurance claims TORONTO – September 23, 2020 – OnCall Health today announced that its premium virtual care platform is being used by HVE Healthcare Assessments to facilitate assessments for insurance companies that require independent, unbiased medical opinions to validate benefits claims. Powered by OnCall Health, HVE Healthcare Assessments offers virtual psychology, psychiatry, […]
OnCall Health raises $6M Series A to enable virtual care programs for healthcare brands

Funding will be used by OnCall Health to expand its reach and build out its software to enable healthcare systems to launch and scale their telehealth operations TORONTO — September 15, 2020 — OnCall Health, a company that provides virtual care software to healthcare providers, today announced it has raised US$6M in Series A funding, bringing the […]
Trafalgar Addiction Centers deliver virtual care rehab program with OnCall Health

TORONTO – July 9, 2020 – OnCall Health today announced that its virtual care platform is being used by Trafalgar Addiction Treatment Centres to offer virtual settings for addiction and mental health treatment. Since the onset of the pandemic, over 60 people have participated in Trafalgar’s Intensive Virtual Addiction Rehab Program from the safety of their homes. Graduates and alumni of Trafalgar’s Residential and […]
OnCall Health teams up with Lumino Health to connect healthcare professionals with virtual care

TORONTO – June 1, 2020 – Today, OnCall Health announced a commercial partnership with Lumino Health, an innovation from Sun Life, to connect healthcare providers with Canadians from a distance. OnCall Health is providing its virtual care software to healthcare providers on the Lumino Health network, Canada’s largest network of healthcare providers. OnCall Health’s simple and secure virtual care software is trusted […]
How telehealth is helping healthcare providers and patients better respond to the coronavirus outbreak

How is Coronavirus (COVID-19) affecting healthcare? Healthcare providers are experiencing major challenges as the Coronavirus disease continues to put pressure on the healthcare system. Many patients are avoiding appointments and doctor’s offices in an effort to prevent a potential exposure to COVID-19 while others are flooding hospital emergency rooms without exhibiting any symptoms. As a […]
Virtual care platform helps Alberta patients with sexual therapy

Alberta’s Insight Psychological is a counselling practice that has implemented a virtual care platform, including videoconferencing and instant messaging, to provide psychological services to Albertans. Sexual therapy is one of Insight’s specialties, with ASSECT certified therapists and sexologists in major cities, including Edmonton and Calgary. Insight works with Toronto-based OnCall Health, a developer of a […]
Overview of Ontario health agencies

The Government of Ontario recently announced changes to the way health care will be ran in Ontario by proposing Bill 74, known as ‘The People’s Health Care Act, 2019’. If passed, the current Ontario health care system will be restructured to form Ontario Health agencies in order to provide a one-point-access of care for patients. […]
How telehealth can save Canadian employers billions of dollars

The Public Health Agency of Canada estimates that chronic diseases cost the Canadian economy $190 billion annually in lost productivity and healthcare costs, and that number is increasing every year. Employers must be proactive with their employees’ health and provide the resources necessary for improved quality of life. Utilizing telehealth for chronic disease management in workplace […]
Are you using HIPAA compliant telehealth tools?

Are you using PHIPA or HIPAA compliant telehealth tools for your healthcare organization? You are constantly looking for ways to better serve your patients. From new telehealth solutions to online technologies so providers can better connect and engage with patients. But are these tools, and how they use and control patient data, PHIPA or HIPAA […]
How telehealth is key to solving the global mental health crisis

Telehealth is key to solving then global mental health crisis Globally, mental illness has become one of the leading causes of illness and disability. It’s estimated that 450 million people suffer from at least one mental disorder, and one person commits suicide every 40 seconds. Unfortunately, mental illness rates are still on the rise and the end doesn’t […]
How telehealth can increase your company’s ROI

How can telemedicine increase your clinic’s ROI What are Telemedicine’s benefits and how can they have a significant impact on your business’ bottom line? Are you considering the costs and benefits of implementing telemedicine in your organization or clinic? A virtual care platform includes tools such as online video appointments, self-booking tools, online payment processing, […]
Addressing Canadian healthcare wait times with telehealth

Addressing Canadian Healthcare Wait Times with a Telehealth App The Canadian healthcare system is often spoken of in a controversial manner, even among Canadians. There are arguments about whether the cost of care, quality of resources and care options, as well as accessibility are up-to-par with other developed countries. Since the Affordable Care Act was […]
Best practices for healthcare staff while using a telehealth platform

Best practices for healthcare administrative staff using telemedicine software As a member of a healthcare organization’s or clinic’s administrative team, administrators are often one of, if not the, first point of contact for new and existing patients. Knowing how to best incorporate telemedicine software means that administrators play an important role in ensuring patients are […]
The ethics of telehealth

The ethics of telemedicine software As a healthcare leader or provider, it can be daunting to introduce new telemedicine software into your organization or clinic. This is especially true if the tools in question have the potential to compromise your organization, decrease access to care, affect operational efficiency, or harm patient relationships. Healthcare leaders and […]
How to introduce telehealth to patients
The most important thing to remember is that introducing virtual care will help streamline your administrative tasks and expand the reach of your services. This should not be an overwhelming or daunting change! The guide below will help you communicate this to your clients. Explain how it works: Keep in mind, virtual care may be […]
OnCall Health raises $2M CAD Seed Round to accelerate adoption of virtual care in healthcare systems

TORONTO, April 16, 2019 – OnCall Health, a platform that provides simple, secure virtual care technology and services for healthcare providers, today announced it has raised $2 million CAD ($1.5M USD) in seed funding to expand its operations in North America. The round was led by Ripple Ventures with participation from Panache Ventures, Stout Street Capital, and Maple […]
